Contents
Abstract
Objective
Consumers are living longer, creating more pressure on the health system and increasing their requirement for self-care of chronic conditions. Despite rapidly-increasing numbers of mobile health applications (‘apps’) for consumers’ self-care, there is a paucity of research into consumer engagement with electronic self-monitoring. This paper presents a qualitative exploration of how health consumers use apps for health monitoring, their perceived benefits from use of health apps, and suggestions for improvement of health apps.
Materials and Methods
‘Health app’ was defined as any commercially-available health or fitness app with capacity for self-monitoring. English-speaking consumers aged 18 years and older using any health app for self-monitoring were recruited for interview from the metropolitan area of Perth, Australia. The semi-structured interview guide comprised questions based on the Technology Acceptance Model, Health Information Technology Acceptance Model, and the Mobile Application Rating Scale, and is the only study to do so. These models also facilitated deductive thematic analysis of interview transcripts. Implicit and explicit responses not aligned to these models were analyzed inductively.
Results
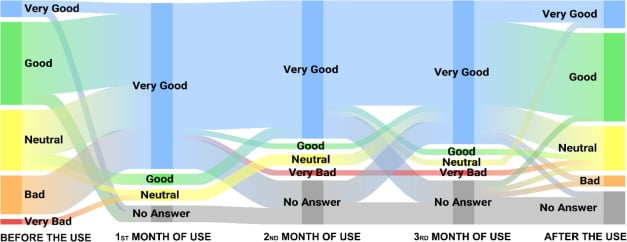
Twenty-two consumers (15 female, seven male) participated, 13 of whom were aged 26–35 years. Eighteen participants reported on apps used on iPhones. Apps were used to monitor diabetes, asthma, depression, celiac disease, blood pressure, chronic migraine, pain management, menstrual cycle irregularity, and fitness. Most were used approximately weekly for several minutes per session, and prior to meeting initial milestones, with significantly decreased usage thereafter. Deductive and inductive thematic analysis reduced the data to four dominant themes: engagement in use of the app; technical functionality of the app; ease of use and design features; and management of consumers’ data.
Conclusions
The semi-structured interviews provided insight into usage, benefits and challenges of health monitoring using apps. Understanding the range of consumer experiences and expectations can inform design of health apps to encourage persistence in self-monitoring.
Introduction
The increasing aging population will benefit from 21st Century self-care techniques, easing burden on healthcare by enabling self-monitoring at home, office or other location.[1] In order for self-care of a chronic condition to be sustained, self-management techniques need to be integrated into one’s life.[2, 3] Due to differences between chronic conditions, there is no agreed definition of self-care.[4] One commonality is that self-care requires self-monitoring for a consumer to pursue daily decisions to maintain functionality.[4] Self-monitoring can be conducted by consumers on various levels; examples are self-awareness of symptoms (e.g. shortness of breath), manual blood pressure readings, and self-maintained electronic databases of blood glucose measurements in diabetes management. For consumers with reasonable health literacy, self-monitoring offers greater autonomy, aiming to reduce pressure on health resources.[5–8]
Despite being a relatively new phenomenon, self-monitoring has experienced notable developments in its practical immersion into one’s lifestyle. Health consumers are increasingly engaging with mobile health applications (‘apps’)[9] for self-monitoring. However, limited regulation in the technology marketplace enables insufficiently tested[10, 11] self-monitoring devices to be launched, with potential for health consumers to ill-advisedly change their self-care regimens. There are many instances of ‘buggy’ health apps.[10, 11] Indeed, a number of authors have called for guidelines around electronic self-monitoring to prevent errors or other incidents.[12, 13] In Australia, the introduction of the Health Market Validation Program[14] signifies the Victorian State Government’s and technology vendors’ commitment to remote/home monitoring; feasibility studies are required in other jurisdictions.
Research incorporating Consumer Experience Metrics
One report, in which consumer experience with health apps was a key outcome, describes two Swiss university randomised pragmatic trials.[15] Both studies explored whether an app-based intervention was more effective than self-management of chronic pain without an app. The apps included modules for participants to write diary entries and complete questionnaires during the six-month intervention. Consumer experience was measured in terms of adaptability and pre-post sick leave,[15] with the Chronic Pain Acceptance Questionnaire[16] used to record sick leave taken by participants.
Consumer experience was also included in a four-week British weight management study involving seven females and six males.[17] A hybrid website and smartphone app were trialed. Semi-structured telephone interviews were used to assess the two platforms, with data analyzed via inductive thematic analysis.[17] Participants noted improvement in self-reported dietary and physical activity. No confounding factors relating to weight management were acknowledged. Key outcomes relating to goal engagement included motivation, self-efficacy, awareness, effort and achievement. The researchers encouraged critique of the app, whereby participants suggested use of barcode scanners and free-text entry boxes.
Since self-care transfers most of the responsibility to the consumer, the usability of technology for this purpose is imperative. Consequently, self-care technologies need to be adaptable to technological environments and user preferences.
A growing number of studies have explored the impact of technological interventions on consumers’ health outcomes. These interventions have included automated reminders (via text messaging)[18, 19] and internet-based information,[20] and have been assessed using self-report by participants,[21] with little, if any, external validation. Poor persistence with long-term self-monitoring is evident in chronic conditions such as asthma.[22] Gamification can be used to increase engagement through use of rewards for repeat logins within a period of time and achieved milestones.[23] With many usability features conceived to date, mobile health app design is constantly evolving;[24] many app development frameworks offer fast, scalable interfaces to deploy changes to user interfaces seamlessly.
An American health app study reported sociodemographic characteristics of app users, through a 36-item cross-sectional survey of 1604 English-speaking adults.[25] At least one health app had been downloaded by 934 of the participants. Data from open-ended questions, such as effectiveness of the app and reasons for halted use, were thematically analyzed by two researchers, and revealed Weight Loss, Calorie Tracking, Nutrition, and Physical Activity as their main themes. While facilitating statistical analysis, large-scale studies are compromised by their limited ability to probe participants for in-depth responses.
Studies into self-care using mobile apps have predominantly involved custom-designed apps. Examples are a pre-post intervention for asthma using the Smart Phone Application,[26] randomised-controlled trials for asthma using the t+ Asthma app[27] and another unnamed purpose-built app,[28] as well as a diabetes randomised-controlled trial using Glucose Buddy.[29] In these studies, self-efficacy was the only measurement of consumer experience, while participants’ engagement with the app was determined via self-report. Engagement does not necessarily mean long-term commitment to using the app; therefore, combining such data with usage statistics, such as login time and frequency and accessed features would add value to these studies. In contrast, mobile app-based obesity management in South Korea[30] applied the purpose-built obesity-management app constructed with ‘knowledge statements’ from an expert committee. Other custom-designed apps include an app for self-monitoring and guiding lifestyle management for breast cancer survivors[31] and PD Dr, a home-based monitoring assessment system for Parkinson’s disease.[32]
Notable deficiencies collectively demonstrated in these studies are their relatively short follow-up periods and lack of detailed consumer experience findings. Additionally, self-management programs have measured select outcomes, rather than a more holistic spectrum of outcomes relevant to conditions such as diabetes, osteoarthritis and hypertension.[4]
Theoretical Frameworks
The Technology Acceptance Model (TAM), published in 1989, quantifies how consumers accept technology.[33] It is an extension of the Theory of Reasoned Action,[34] and is used to predict intended behaviour, adopting a technology-focussed paradigm in decision-making.[35] The TAM has been applied in qualitative[36] and quantitative[37] studies of health apps to determine the acceptance of mobile technology amongst physicians and medical students, respectively, and in health-related studies on topics such as adoption of health apps.[38]
The Health Information Technology Acceptance Model (HITAM) is an evolution of the third version of the TAM for the health technology field,[39] combining behavioural, personal, social and IT factors. This model also embraces the Health Belief Model[40] and has been used in asthma studies for investigation of medication compliance.[41, 42] However, no literature was found in which the HITAM informed research into the use of health apps.
The Mobile Application Rating Scale (MARS) is a validated and reliable scale[43] due to its internal consistency, inter-rater reliability and comprehensive extraction of 25 papers and resources in its formation. The MARS is an Australian development from 2015 to assess the quality of health apps, and is based on four quality scales: engagement, functionality, aesthetics and information quality. Research applying the MARS in studies involving health apps is emerging, with MARS noted in an Australian wellbeing evaluation protocol[44] and mentioned in an Irish mental health app feasibility study without being used in the study itself.[45]
Other theoretical models and frameworks have been applied in studies of self-care. The PRECEDE-PROCEED model has been applied in an asthma study in Taiwan[46] to measure factors such as asthma knowledge and self-efficacy; this model contains elements such as administrative and financial policies that may not be relevant to exploratory research.[47] Similarly, Orem’s Self-Care Model has been applied to asthma to investigate “self-care abilities, self-care practices, and health outcomes.”[48] However, this model and the PRECEDE-PROCEED model lack consideration of technological factors.
Review of the literature suggests the TAM, HITAM and MARS are the most relevant frameworks to qualitatively explore consumers’ experiences of mobile health apps. While no published research has applied a combination of these models, integration of the TAM, HITAM and MARS should improve cross-disciplinary relevance and robustness, and provide theoretical grounding for exploratory research into the consumer experience with health apps.
The objectives of this study were therefore to 1) qualitatively explore consumers’ experiences with mobile health apps and 2) their perceived benefits from use of health apps, and 3) formulate suggestions for improvement of health apps.
Materials and Methods
This study explored consumers’ experiences with health apps through semi-structured interviews. The Human Research Ethics Committee of Curtin University approved this study (approval number RDHS-102-15). In accordance with this approval, participants provided signed informed consent for interview.
Inclusion criteria were minimum 18 years of age (no maximum), residence in the metropolitan area of the University (for convenience), conversational fluency in English, and recent (at least one month’s) experience with any health/fitness mobile app. Any duration of use of the app(s) was of value, because discontinued use and negative experiences complemented data from persistent users. It was intended to involve participants of a broad age range to combine experiences of the tech-savvy younger generation with the older generation.
Including fitness apps enabled participants with chronic conditions such as obesity, diabetes and high blood pressure to elaborate on their experiences without restricting them to disease-specific apps. Participants without a chronic condition were included to capture fitness app usage amongst chronic disease consumers and healthy counterparts.
Guiding the research was the post-positivism worldview where relationships can be reverse-engineered via tested approaches such as deductive analysis.[49] A reductionist philosophy was applied to deconstruct implicit and explicit responses into manageable variables. The qualitative paradigm was crucial to appreciate, observe and deduce consumers’ experiences. The use of individual interviews offered privacy, and enabled exploration of each user’s interaction with their identified health app(s). Semi-structured interviews provided participants freedom to elaborate on the interview guide (Table 1).
Constructs of the TAM,[33] specifically, perceived ease of use and perceived usefulness, were included in the interview guide. The HITAM included constructs describing personal and social factors such as motivation, self-reflection, competition and recommendation. Additionally, features of the MARS, such as engagement and aesthetics, were included. Duplicated concepts between the three models were deleted. Questions were adapted to suit this study, with the interview guide comprising core questions and supplementary questions for clarification and elaboration. The supplementary questions reflected “acceptance factors of mobile apps,”[51] collectively capturing all perceivable aspects of consumers’ health app usage. Following independent review of the draft interview guide, the structure was revised to enable participants to reflect on more than one app during the interview.
Participants were a convenience sample of residents in the Perth metropolitan area, aged 18 years or older and conversationally fluent in English, who self-reported recent use of any commercially-available health/fitness app with capacity for self-monitoring and data input. Any duration of use was included, because discontinued use and negative experiences were considered to provide valuable insights into persistence, and complemented data from persistent users. No preferential sampling of participants with either negative or positive experiences was applied.
A multi-faceted recruitment strategy was applied. Participants were recruited via co-operation with health associations such as Celiac Australia and Diabetes Australia, through their social media accounts and eNewsletters over a period of four weeks. A local radio station popular with a mature demographic was also utilized in an attempt to recruit listeners with an interest in self-care. The first author’s affiliation with a technology start-up hub enabled a broadcast announcement to members to attract participants from different educational backgrounds who shared a common goal to innovate. A static text advertisement was posted on the University portal, in addition to posters with a Quick Response Code at shared university computer workspaces and the library.
Interviews were scheduled in quiet locations such as a public library or participant’s office. A single interviewer (author KA) conducted all interviews in June and July, 2015. The first several interviews were used to reflect on the question guide. Interviews were digitally recorded, supplemented with field notes and post-interview reflections. Data saturation was perceived through recurring explicit ideas[51] such as motivation, customisation, interconnectivity, data inaccuracy, convenience and competitiveness, and confirmed during analysis. Literature suggests 20–25 participants ranging generally provides adequate saturation of themes when using qualitative semi-structured interviews.[54–56] Advertising was halted after four weeks on-campus and seven weeks off-campus. Audio files were professionally transcribed by an accredited agency with privacy certification. Raw data files were imported to QSR NVivo 10 for open coding and analysis.
Braun and Clarke’s six-step thematic analysis approach was utilised to capture user experience themes,[57] addressing Objective 1. The deductive approach[58] was applied to continually reflect on, and refine, emerging themes. The deductive coding framework was synthesized using the TAM, HITAM and MARS. Step One involved data familiarization to verify accuracy of transcriptions. This required the researcher to become intimate with the transcripts by re-reading them and referring to field notes. As per Step Two from Braun and Clarke, co-authors confirmed selection of codes and themes, and amendments were made as necessary to reach consensus. Initial coding was performed in NVivo based on the deductive coding framework, with miscellaneous responses interpreted inductively into new codes as required. Two authors matched initial coding to ensure consistency and establish common ground to confirm definition of the full set of themes. Step Three involved clustering nodes to a common theme(s) based on coherent patterns. To ensure robustness, data extracts are quoted in the Results section to demonstrate legitimacy of the identified themes.[57] Step Four involved reduction of themes into most prevalent implicit and explicit ideas.[57] Redundant themes derived from the three published models were deleted. Step Five involved describing the parameters of, and naming, the themes, whilst Step Six involved reporting to convey the analysis made. Outcomes from Steps Four, Five and Six are reported in the Results.
Data are presented based on emergent themes from thematic analysis, exploring how health consumers use apps for health monitoring (addressing Objective 1). Perceived benefits from use of health apps (addressing Objective 2) and suggestions for improvement of health apps (addressing Objective 3) are presented descriptively.
Results
Description of Participants
The most common age bracket of participants was 26–35 years; one participant was over 50 years and another recently turned 18 years old; further participant demographics are provided in Table 2. Interviews were completed in 20 minutes on average, during which time, most participants answered all questions relevant to their experience.