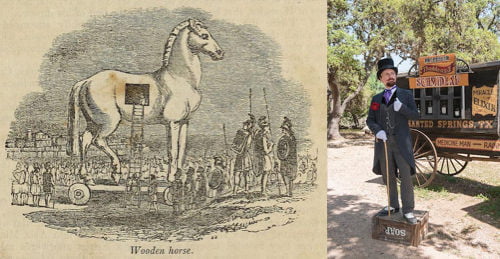
Were digital health innovators best described as a clever Trojan Horse this quarter, or as slimy snake oil salesmen? It really depends on who you ask.
At the beginning of the quarter, HHS CTO Susannah Fox said that technology would be a Trojan Horse for culture change in healthcare. She spoke about the ways HHS is enabling the democratization of technology innovation through the internet.
Later in the quarter, though, the speech everyone was talking about was from American Medical Association CEO Dr. James Madara, who said some direct-to-consumer digital health tools were like snake oil, and the industry still lacked the infrastructure to pick out the good stuff.
Plenty of digital health movers and shakers offered rebuttals, including a few of the speakers at MobiHealthNews’ inaugural event in June. Both CareMore CEO Dr. Sachin Jain and Kaiser Permanente Chief Medical Information Officer Dr. John Mattison saw Madara’s words as a call to action to improve the state of efficacy in the space.
Provider news this quarter spanned a range of categories, from patient engagement to remote monitoring. Read on for the MobiHealthNews provider roundup for Q2 2016.
Telemedicine: Critical scholarship, regulatory ups and downs, and overall growth
One of the most talked about telemedicine stories was a small study in JAMA Dermatology which found that direct to consumer dermatology telemedicine services are lacking in a number of areas, including transparency, diagnostic and therapeutic quality, and thoroughness.
Services offered users prescriptions in 65 percent of the diagnosed cases, but in 32 percent of the cases where users received a prescription, relevant adverse effects were not disclosed. And in 43 percent pregnancy risks weren’t disclosed. Just 26 percent of the services disclosed information to patients about clinician licensure. Some of these services even used a physician based outside the US who didn’t have a California license. Some 23 percent of the services collected the name of the user’s primary care physician and even fewer, 10 percent, offered to send records to the user’s primary care physician.
That wasn’t the only study that came out this quarter critical of telemedicine. A systematic review published in the International Journal of Chronic Obstructive Pulmonary Disease found that there is little evidence that telemedicine interventions consistently improve the quality of life of COPD patients. Researchers looked at 47 studies of telemedicine use in COPD since 2000 and analyzed 18 that met their inclusion criteria. Of those, just three showed a statistically significant improvement in quality of life.
All that said, telehealth adoption continued to rise. According to a small KPMG survey that came out in May, 25 percent of providers have implemented telehealth and telemedicine programs that are financially stable and improving efficiency.
At the American Telemedicine Association conference in May, the CEOs of both Teladoc and American Well spoke about their plans to add chronic condition-focused telehealth to their existing primary care and behavioral health options. While American Well CEO Roy Schoenberg’s comments didn’t pinpoint a timeline, Teladoc CEO Jason Gorevic said they planned to launch the product by year’s end.
American Well’s big announcement at ATA was the launch of The Exchange, a new enterprise telehealth services that will allow payers and providers who use white-labelled American Well telehealth services to offer their care to one another.
Under the Exchange, participating insurer services will be able to negotiate directly with participating provider networks, allowing payers to give their patients access to a wider range of care providers, while health systems have the opportunity to see many new patients. The starting partners are Cleveland Clinic, Nemours Children’s Hospital in Florida, and LiveHealth Online, the American Well-powered telehealth system for Anthem Blue Cross Blue Shield.
Notably, Cleveland Clinic began to experiment with using telehealth to make its doctors more broadly available before ATA, partnering with CVS Minute Clinics via American Well earlier this year.
In its Q1 earnings call, Teladoc reported that it pulled in $26.9 million in revenue, up 63 percent from Q1 2015. Of that total, $20.7 million was from subscription fees and $6.2 million was from visit fees. This year visit fees are made up a larger piece of the pie than last. Teladoc completed 239,942 visits in Q1, up 61 percent from the 148,696 visits conducted in Q1 2015. The company also added 2.9 million new members during the quarter.
Speaking of Teladoc and American Well, the quarter also saw movement in the patent fight between the two, when Massachusetts federal judge Indira Talwani ruled that American Well’s telehealth patents, which the company had sued Teladoc for allegedly infringing, were unenforceably broad. She cited the same Supreme Court precedent, Alice v. CLS Bank, that an ITC judge used to invalidate Jawbone’s patents the month before in the tracker company’s battle with Fitbit.
Last but not least in the world of telehealth, we saw some progress on various legal regulatory fronts.
In Texas, lobbyists for groups affiliated with both telemedicine companies and physician organizations met in a closed-door session to discuss “modernizing our telemedicine statutes and reducing the regulatory footprint governing the provision of telemedicine services,” according to an email that went out to participants. Representatives for the Texas Academy of Family Physicians, the Texas Medical Association, and the Texas e-Health Alliance were all in attendance.
After a long delay, the American Medical Association reconsidered proposed ethics guidelines for telemedicine and ultimately passed them. The guidelines recommend that physicians inform patients about the limitations of these services and encourage them to let their PCPs know about any online visits they’ve had. Professionalism should be up to the same standards as in-person interactions, and physicians should tailor informed consent processes so they work effectively via telehealth services. Physicians should take steps to promote continuity of care for the patients they see via telemedicine technologies and they should work with professional organizations (like the AMA) to help improve telemedicine services and develop clinical standards.
An interesting regulatory drama played out in South Carolina over online eye exams. The state’s legislature passed a bill that that would prevent South Carolina residents from obtaining a glasses or contact lens prescription based on an online eye exam. Governor Nikki Haley vetoed the bill, citing its anticompetitive effect. But the legislature overturned the veto with near-unanimous votes from both houses.
Finally, though not quite a telemedicine story, the quarter also saw a reversal from the Joint Commission, which will now allow health organizations to send orders of care via secure text messaging services. As the third quarter began, the JC moved to delay the rollout of the new rule, however.
Patient-generated health data
Patient-generated health data was a major focus at our inaugural MobiHealthNews event this quarter because it is one of the most important provider trends happening today.
At MHN 2016, Ochsner Health’s Dr. Richard Milani shared how his health system was able to get a little over two-thirds of their out-of-range hypertension patients within range in 90 days by having those patients measure their blood pressure once a week with a connected device. CareMore CEO Dr. Sachin Jain, Dr. Ricky Bloomfield of Duke Health, and a panel that included representatives from Carolinas Health and Dignity Health all weighed in on the topic.
This was also the quarter in which doctors at an emergency room in New Jersey used data from a patient’s Fitbit activity tracker — which they happened to notice on his wrist — to determine his course of treatment. The case study caused quite a stir in the digital health industry, with some saying it demonstrated the value of the technology and others saying the doctors got lucky that using a non-FDA-cleared device in a clinical context didn’t end badly.
But plenty of clinical researchers are using Fitbits in various contexts, as the Q2 publication of part 2 of our Fitbit-in-clinical-trials roundup demonstrated. One of those was a trial at Dana Farber Cancer Institute, which partnered with Fitbit to launch a two-year randomized study that will investigate the impact of weight loss on breast cancer recurrence. The study, called the Breast Cancer Weight Loss (BWEL) study, is sponsored by the National Cancer Institute and the Alliance for Clinical Trials in Oncology.
In April when Columbia University launched a 300-patient RCT to test AliveCor’s Kardia ECG in patients with atrial fibrillation. The study, set to be completed by August 2018, uses AliveCor’s Kardia mobile device, which takes the form of a smartphone case with two electrodes attached to the back. One-hundred and fifty of the 300 patients will be given AliveCor devices and instructed to submit an ECG reading daily for six months. They will also receive HIPAA-compliant text messages to encourage healthy behavior.
Later that month, Dignity Health conducted a 495-patient study of Propeller Health’s connected inhaler. Patients were split into a routine care group and an experimental group. Both had Propeller sensors affixed to their short-acting beta antagonist (SABA) inhalers, which is a rescue inhaler used only when the patient’s asthma becomes exacerbated, but for the routine care group, neither the patient nor their provider had access to the data from the sensor, whereas the intervention group received feedback about where and when they were using the inhaler.
At the end of the study period, both groups had decreased their SABA use and increased their number of SABA-free days, but the intervention group had done so by a significantly larger margin. The study also looked at asthma control at the end of the study, as measured by the asthma control test. For patients whose asthma was well controlled at the start of the study, there was no difference between the two groups. But for patients who began the study uncontrolled, they were more likely to improve with access to the Propeller data.
At the American Telemedicine Association conference in May, remote patient monitoring company Sentrian shared some results from a recent 6-month pilot with Anthem subsidiary Caremore. The Sentrian Remote Patient Intelligence platform uses biosensors to monitor patients remotely, but the company uses machine learning to customize the alert parameters for each patient. When they set the initial parameters, determined by CareMore physicians, they were predicting 60 to 70 percent of COPD hospitalizations, with a high number of false positives, Kriendler said. After six months of machine learning, they’d created an algorithm that detected 88 percent of hospitalizations five days in advance, with only a 3 percent incidence of false positives.
In June, Southern Hills Hospital in Nevada completed a pilot of a technology that used Samsung tablets and a wearable EEG reader to assess patients’ pain and to attempt to lessen that pain with distracting content. The pilot, a collaboration between Samsung, tech company AccendoWave, and Southern Hills, equipped nearly 1,000 ER patients, including adults and children, with Samsung Galaxy tablets, modified using the Samsung Knox toolkit, and EEG reading headbands. Out of the nearly 1,000 Southern Hills patients who used the technology, 90 percent enjoyed using it, 81 percent said it improved their comfort level, 77 percent felt it accurately understood their level of discomfort, and 87 percent reported that they enjoyed the content they were shown.
A few more developments that could pave the way for future remote patient monitoring news: Towards the end of the quarter, Nokia Technologies announced that it would work with Helsinki University Hospital (HUS) and the University of Helsinki to develop new technologies for outpatient care, starting with remote patient monitoring solutions and the FCC appointed the Enterprise Wireless Alliance to serve as frequency coordinator for Medical Body Area Networks (MBANs). The EWA launched a website where healthcare facilities can register MBANs, signaling that the creating of that spectrum is coming very soon.
Patient engagement, hospital apps, and a little bit of virtual reality
Two pieces of patient engagement news this quarter came from the Office of the National Coordinator for Health IT. First, the ONC received an open letter from the Consumer Partnership for eHealth (CPeH), a non-partisan coalition led by the National Partnership for Women and Families, who argued that interoperability and information exchange won’t truly be complete until they include the patient and their family caregivers. In the letter, CPeH notes that patient engagement is already a part of ONC’s Interoperability Roadmap. They argue against segmenting patient access to records and provider access to records, or prioritizing one over the other.
Around that same time, ONC launched two new online tools to connect patients to their data, a series of consumer-facing videos to educate patients about their data access rights and a provider-facing “Patient Engagement Playbook” to walk hospitals through the steps to patient engagement. On the access website, ONC describes it as an “evolving resource”, suggesting that the agency will continue to add to and adapt the playbook.
Most of the patient engagement news this quarter though, was focused on hospitals launching or testing out different patient-facing apps.
For instance, late in the quarter Mount Sinai Health System (MSHS) in New York launched MountSinaiNY, a new patient-facing app that the health system says will serve as an umbrella app for current and future patient-facing apps their team launches. Mount Sinai partnered with San Jose, CA-based LifeMap Solutions, a subsidiary of BioTime, to develop the app.
In April, Yale School of Medicine researchers announced plans to launch a new app, called Hugo, in partnership with Yale New Haven Health System, that allows patients to collect health data and participate in studies by sharing that data with researchers.The app will organize the data that it collects and then sync this data with a research database.
Boston Children’s hospital launched an interesting piece of software, but it wasn’t a smartphone app. The hospital launched an app for Amazon Echo. KidsMD gives the voice-powered home appliance a new “skill” that will allow it to give simple health advice to parents about their children’s’ fever and medication dosing. The Alexa app is just the first step in a plan to bring Boston Children’s medical knowledge to the consumer space, according to Chief Innovation Officer John Brownstein. Boston Children’s also piloted Crisis Care, a suicide prevention app for teens and their parents, and shared data from that pilot at an event in Boston this past quarter.
A couple of hospitals tested out apps from third-party vendors. Baltimore, Maryland-based Everseat, which offers an app and website that helps patients schedule doctor’s appointments, inked a deal with rideshare company Lyft to help people get to their doctor’s appointments. Everseat also recently added Beth Israel Deaconess Medical Center in Boston as a customer. BIDMC is piloting Everseat’s scheduling service in a handful of practices so far: dermatology, orthopaedics, pain management, physical therapy and rehabilitation. And, also in Boston, Brigham and Women’s Hospital tested Medisafe’s medication adherence app in a randomized control trial of 390 patients taking medication for high blood pressure.
Speaking of apps, the latest attempt to create an app curation platform, a website from MIT’s Hacking Medicine Institute, also launched this quarter.
UCSF and Stanford both approached patient engagement via virtual reality. At UCSF, Center for Body Computing Executive Director Dr. Leslie Saxon shared how the team is creating virtualized versions of their doctors. She sees virtualized physicians as a way to maximize meaningful time spent with patients and make sure healthcare resources are used efficiently and patients practice at the top of their license.
And in May, MobiHealthNews learned that The Stanford University School of Medicine and the Stanford Virtual Human Interaction Lab will collaborate on a small clinical trial investigating the possibilities for virtual reality in treating conversion disorder. Participants will use special software developed by the VHIL, combined with the Oculus Rift, to inhabit a virtual avatar body.
What’s new with Apple and Google?
Though they didn’t dominate the news cycle as much as they have in past quarters, Apple and Google both made some news particularly relevant to healthcare providers.
Apple, of course, launched CareKit, the follow up to HealthKit and ResearchKit, at a special event in March. In April the CareKit framework went live and Apple announced that Cleveland Clinic would be an early adopter, using the CareCard and Insights Dashboard modules of CareKit to build an app that will help patients track their symptoms and engage with their health.
The iOS10 updates announced at Apple’s WorldWide Developer Conference brought some more Apple health updates, including news that Apple HealthKit would add support for the HL7 Continuity of Care document.
Researchers from a number of universities, including the University of Nebraska, University of Michigan, Vanderbilt, Northeastern, and Wake Forest University, launched a new ResearchKit study to explore questions about cognitive function in people with Alzheimer’s disease. Also in the quarter, the Robert Wood Johnson Foundation announced a $500,000 challenge to design a mood-related ResearchKit app. New Venture Fund and Luminary Labs are also supporting the challenge.
At its Google IO event, Google announced a new version of its Android Wear software, called Android Wear 2.0, and two fitness-related updates: automatic activity tracking and a Google Fit data exchange API. Apps can now exchange data using the Google Fit API, so data like calories consumed in a nutrition app can sync with calories burned in a running app. This kind of fitness and health data exchange was a feature Apple’s HealthKit launched with in 2014.
Google also entered into a content partnership with Mayo Clinic and Harvard Medical School to improve its search function for health-related content, specifically symptom searches.
There was also a little bit of Google Glass news this quarter. (Reports of the technology’s death are apparently exaggerated). Google Glass startup Augmedix raised a strategic round of $17 million and the investors included a number of hospitals: Sutter Health, Dignity Health, Catholic Health Initiatives (CHI), TriHealth Inc. and one other which chose to remain anonymous.
Another Google Glass startup, CrowdOptic, announced its first integration with Cisco’s team communications app Jabber. Physicians at the UCSF Medical Center at Parnassus will be able to access Cisco Jabber through their smart glasses, using CrowdOptic software. The technology can be used for real time virtual consults or to livestream surgeries or other procedures, in order to train surgeons and medical students.
[Source:- Mobi health News]